A retrospective analysis from data in a study from Japan indicates that initiating anti-vascular endothelial Growth Factor (VEGF) treatment before best corrected visual acuity (BCVA) declines and advanced lesions develop would afford better visual outcomes for eyes of patients with age-related macular degeneration (AMD). They also found that eyes with a relatively good initial BCVA, such as < 0.3 in logMAR (Snellen 20/40), and without fibrovascular PED would achieve sustained or improved BCVA after anti-VEGF treatment within 3 years of follow-up.
This paper, published in Journal of Clinical Medicine, retrospectively reviewed visual outcomes of eyes with AMD treated with anti-VEGF drugs in a real-world setting. This study, from the Department of Ophthalmology, St. Luke’s International Hospital, and Department of Ophthalmology, Keio University School of Medicine, both in Tokyo, Japan, involved all patients who received anti-VEGF treatment as the first therapy for AMD, and were followed up for at least 12 months and up to 36 months, including those who dropped out during the study period; patients who dropped out were included in Kaplan–Meier survival analysis, which may more precisely reflect real-world conditions of the daily clinical practice.
 |
| (c) Journal of Clinical Medicine |
Treatment failure was defined as a BCVA reduction ≥ 0.2 of logMAR compared with the initial BCVA at each time point. Failure was also considered when patients received treatment other than anti-VEGFs. Survival or failure was determined every 6 months after the initial anti-VEGF treatment.
Since you’re here...we have a small favor to ask. Retina Global is a nonprofit, and we have to depend on your support to sustain the work we do. Hence the need to ask for your help. Retina Global's work is important, since it not only provides help to disadvantaged people, but also provides resources for developing new treatments that can potentially cure blindness. What we do takes a lot of time, money and hard work. But we do it because we believe we have to help stop someone somewhere from going blind. So make a difference. Click here to donate. Your support is much appreciated. Thank you!
For the 104 eyes of 104 patients with AMD, the mean age was 73.8 ± 1.1 (range, 50 to 93; median, 77) years, and 69 (66.3%) of the patients were men. Eighty-five eyes (81.7%) were categorized as having polypoidal choroidal vasculopathy, thirteen eyes (12.5%) had typical AMD, and seven eyes (6.7%) had retinal angiomatous proliferation.
The mean BCVA was 0.444 ± 0.052 (range, −0.176–2.3; median, 0.301) in logMAR, and the mean central retinal thickness measured in the OCT images was 356 ± 16 μm (range, 102–911 μm; median, 309). The mean BCVA at the final visit was 0.360 ± 0.049 (range, −0.176–2.0; median, 0.155) in logMAR, and there was significant improvement according to the Wilcoxon rank sum test (p = 0.012). Maintained or improved BCVA at the final visit ≥ 0.2 in logMAR compared with initial BCVA was observed in 93 eyes (89.4%).
The mean injection number was 7.5 ± 0.5 (range 1 to 22).
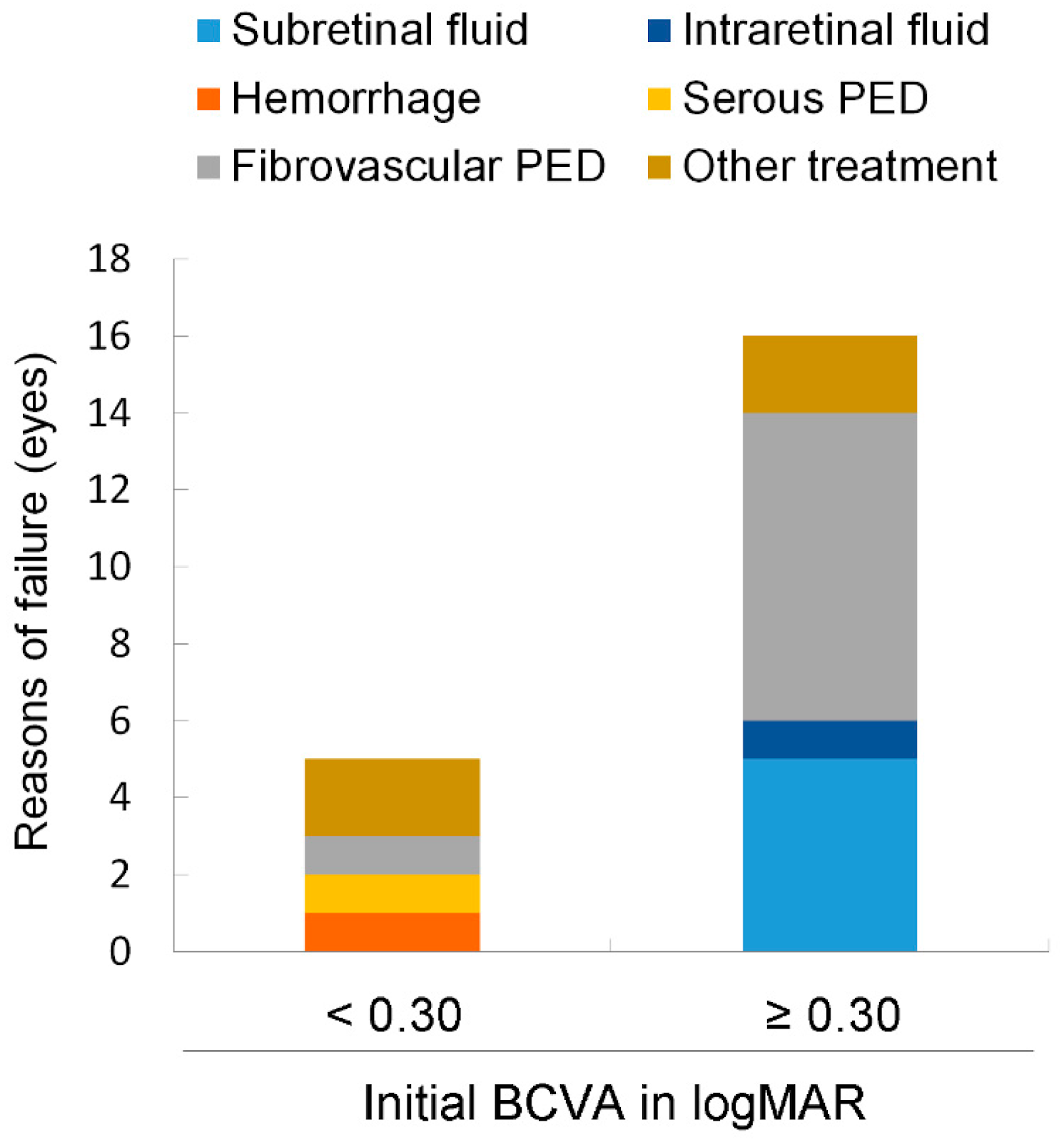
Among the 104 eyes of 104 patients with neovascular AMD who were followed up for at least 12 months and up to 36 months, the median initial BCVA was 0.3. According to logistic regression analyses adjusted for age, having an initial BCVA < 0.3 in logMAR was a positive predictor, and the initial presence of fibrovascular PED was a negative predictor of maintained or improved BCVA at the final visit after anti-VEGF treatment. Kaplan–Meier survival analysis showed that the eyes with an initial BCVA < 0.3 in logMAR had a better survival rate than the others when failure was defined as a BCVA reduction ≥ 0.2 from the initial BCVA at each time point up to 36 months. Eyes with an initial BCVA < 0.3 in logMAR belonged to younger patients; more frequently exhibited SRF; and less frequently exhibited IRF, submacular hemorrhage, and fibrovascular PED at baseline.
The presence of fibrovascular PED at baseline was a risk factor for BCVA decline after anti-VEGF treatment. Fibrovascular PED was also a major reason for visual loss, and eyes with worse BCVA (≥ 0.3 in logMAR) more frequently had fibrovascular PED.
Intraretinal fluid (IRF) was not a significant predictive factor for the risk of treatment failure, although the presence of initial IRF was related to worse BCVA at baseline.
Authors conclude that eyes with a relatively good initial BCVA, such as < 0.3 in logMAR, and without fibrovascular PED would achieve sustained or improved BCVA after anti-VEGF treatment within 3 years of follow-up in the real-world setting. Early treatment would be recommended for exudative AMD, although further studies are required.

So are you suggesting screening asymptomatic patients with Amsler grid testing or OCT. That places a burden on techs and ophths..
ReplyDelete